by John L. Wilson.
The Germ Theory

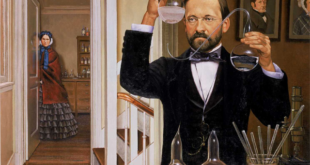
In the summer of 1856 M. Bigo came to consult Pasteur concerning the difficulty he was having with the alcoholic fermentation of beet sugar in his distillery. Something was going wrong with the process and the alcohol was turning sour. Pasteur was at first hesitant to undertake a project outside his school. Fortunately for posterity he decided to go to Mr. Bigo’s distillery and have a look at his vats. He found that, part of the time and for no apparent reason, the alcoholic fermentation process for which yeast was the ferment began to produce lactic acid, an acid usually obtained from sour milk. Pasteur decided that there were in fact two kinds of fermentation, each independent of the other, going on in M. Bigo’s vats: alcoholic fermentation due to yeast and lactic acid fermentation due to the lactic acid bacillus. When the alcoholic fermentation turned sour it was due to the production of lactic acid by a contaminant, the lactic acid bacillus. Pasteur discovered and isolated the bacillus, and believed that the air was the source of the contamination.
Hitherto, fermentation had been described in all the textbooks as a chemical process, but Pasteur had now shown it to be caused, in the case of lactic acid fermentation, by a living organism. Skeptical also of the chemical theory of alcoholic fermentation, he went on to disprove the theory by demonstrating that yeast is the living agent of the process. He reported his findings in a “Mémoire sur la fermentation appelée lactique” (Memoir on the fermentation of lactic acid) in 1857, and a “Mémoire sur la fermentation alcoholique” (Memoir on the fermentation of alcohol) in 1860. Pasteur’s experiments proved conclusively that fermentation is caused by microorganisms. In so doing, he provided a biological explanation for a phenomenon generally accepted as a chemical reaction. Furthermore, he established that specific microorganisms are responsible for specific biological processes and, by inference, that specific germs may be the agents of specific diseases. While Pasteur thus laid the foundation for the germ theory of disease, validation of the theory awaited the test of clinical application soon to be undertaken by the British surgeon, Joseph Lister.
Doctrine of Spontaneous Generation
Pasteur knew that his concept of biological activity by microorganisms was incompatible with the doctrine of spontaneous generation that still had many adherents. In his day the belief persisted that microscopic life forms could be spontaneously generated in putrefying organic material. According to this theory, the microorganisms associated with fermentation were the product and not the cause of the process.
The ancient and hardy doctrine of spontaneous generation, rooted in the speculations of the Greek philosopher Aristotle of the fourth century B.C., was strongly supported by Félix Archimède Pouchet (1800-1872), Director of the Museum of Natural History in Rouen, a French city northeast of Paris. In a paper read before the Paris Academy of Sciences in 1858 he claimed to be able to produce spontaneous generation at will in a sterile culture medium. Pasteur, unerring in his sense that this stubborn doctrine required the coup de grace as only he could administer it, was unwilling to let Pouchet’s claim go unchallenged. Therefore, he began an extensive series of meticulous experiments in 1859, the year of Darwin’s publication of the Origin of Species – and the year that saw the opening of the first medical school on the Pacific Coast by Elias Cooper. Pasteur’s experiments took him from the crowded streets of Paris to the Alps, gathering samples of air in glass flasks containing sterile culture medium. There was rigorous attention to every detail. Flasks opened in the Paris streets grew organisms abundantly, those opened in the high mountains remained sterile with rare exception. To his own satisfaction, and that of the l’Académie des Sciences, Pasteur demonstrated that microorganisms appeared in flasks of sterile culture medium only when contaminated by exposure to contaminated air from the outside, and never by “spontaneous generation.” In 1861 he summarized his findings in the essay Sur les corpuscules organisés qui existent dans l’atmosphère. Examen de la doctrine des générations spontanées. (On the organized bodies which exist in the air. Examination of the doctrine of spontaneous generation.)
Pasteur considered the matter closed. Nevertheless, the dispute dragged on and we can detect his exasperation in the tone of his lecture at the Sorbonne in 1864 when he outlined the history of the controversy and concluded by saying:
Gentlemen, I could point to that liquid (in the flask of sterile culture medium on the table before him) and say to you, I have taken my drop of water from the immensity of creation, and I have taken it full of the elements appropriated to the development of inferior beings. And I wait, I watch, I question it, begging it to recommence for me the beautiful spectacle of the first creation. But it is dumb, dumb since these experiments were begun several years ago; it is dumb because I have kept it from the only thing man cannot produce, from the germs which float in the air, from Life, for Life is a germ and a germ is Life. Never will the doctrine of spontaneous generation recover from the mortal blow of this simple experiment.
No, there is now no circumstance known in which it can be affirmed that microscopic beings came into the world without germs, without parents similar to themselves. Those who affirm it have been duped by illusions, by ill-conducted experiments, spoilt by errors that they either did not perceive or did not know how to avoid.
Meanwhile, Pouchet continued to generate life in his “sterile” cultures. As a result, doubts of Pasteur’s thesis lingered until 1876. By this time Pasteur and his associate, C. Chamberland, had discovered that some bacteria have a resting spore stage during which they are resistant to the temperatures then used in sterilizing experimental cultures. They showed that, in the experiments of Pouchet, the presence of resistant spores in their hay infusion cultures accounted for the subsequent growth. By heating these cultures to 115-120 degrees centigrade, Chamberland destroyed the spores and sterility could be universally maintained in the infusions so treated. The age-old doctrine of spontaneous generation was finally demolished.
Pasteur’s seminal contributions are by no means limited to germ theory and spontaneous generation. His other memorable works include the following and many more: identification of the microorganisms responsible for contamination of wine (1863) and for diseases of silkworms (1865); identification of the bacteria causing gas gangrene (Clostridium septicum), furunculosis (Staphylococcus) and puerperal fever (Streptococcus). He showed that the spoiling of wine by living microorganisms could be prevented by heating for about 30 minutes at 68 degrees C. (154.4 degrees F.), a process now known as pasteurization and widely used in the preservation of milk and other liquids. His last and one of his greatest works was on rabies and vaccination for the prevention of rabies and other conditions. These investigations led to the discovery of the principles of acquired immunity and practical methods of producing it by artificial means.
Joseph Lister (1827-1912)
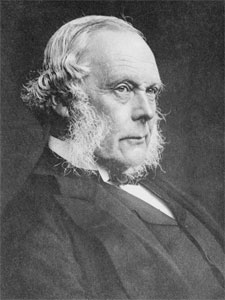
The British surgeon, Joseph Lister, was the first to demonstrate the medical significance of Pasteur’s work on fermentation and spontaneous generation. Pasteur demonstrated by his experiments that living germs are widely distributed in the air and are the agency of fermentation and putrefaction. When Lister read Pasteur’s papers in the early 1860’s, he concluded that the inflammation, “laudable pus” and “putrid intoxication” which commonly followed open wounds, was caused by microbes from the air and surrounding surfaces.
Lister was well suited for the task of evaluating this new conception of the origin of wound infection, the dreaded nemesis of surgeons. He was born at Upton in the county of Essex of Quaker parents who engendered in him the creed of devotion to the good of mankind, with kindness and consideration for others. His father, a wine merchant, devoted his leisure to optics and made important contributions to modern microscopy through improvements in achromatic lenses. Exposure to microscopy under his father’s tutelage was an early preparation for the important research in microbiology he conducted in later life. The young Lister graduated in Medicine at the University of London in 1852, and in 1854 went up to Edinburgh to study surgery with the distinguished James Syme, whose daughter he married. In 1860, on Syme’s recommendation, Lister competed successfully for the chair of surgery at Glasgow, a post he held until 1869. He then returned to Edinburgh where he succeeded Syme and remained until, in 1877, he accepted the position of Professor of Clinical Surgery at King’s College, London. There he stayed until his retirement, replete with honors, in 1892. [142] In 1897, Lord Lister became the first medical man to be elevated to the peerage.
It was during his tenure as Professor of Surgery at Glasgow from 1860 to 1869 that Lister developed and put to trial the principles of “antiseptic surgery” based on the theory that wound infection could be prevented by destroying with an antiseptic the bacteria in the air, on the skin and other surfaces, and in the wound. After evaluation of various bactericidal agents he chose carbolic acid as most effective for this purpose, including its use as a spray before each operation to kill the microbes in the air. (In 1890 he discontinued the spray, having concluded that it was not an essential.) The initial procedures devised by Lister were cumbersome and the carbolic acid was irritating to the patient’s skin and wound and to medical personnel. He gradually succeeded in minimizing these drawbacks by diluting the carbolic acid and experimenting with various types of antiseptic dressing. By 1865 he was prepared to treat patients, beginning with such cases as compound fractures and chronic (tubercular) abscesses, then moving on to amputations.
Two years later Lister’s first paper on the antiseptic method, published in the Lancet in early 1867, dealt with trials of the method in patients with compound fractures, and included a preliminary report on its prevention of secondary infection when draining tubercular abscesses. [146] The results fulfilled his “most sanguine anticipations.” In reality, the results could not have been more striking, for the patients suffered neither from inflammation and abscess in the wound nor from general sepsis, complications expected to occur frequently in such cases. In the introductory section of the paper, he graciously acknowledged his debt to Pasteur:
Turning now to the question how the atmosphere produces decomposition of organic substances, we find that a flood of light has been thrown upon this most important subject by the philosophic researches of M. Pasteur, who has demonstrated by thoroughly convincing evidence that it is not to its oxygen or to any of its gaseous constituents that the air owes this property, but to the minute particles suspended in it, which are the germs of various low forms of life, long since revealed by the microscope, and regarded as merely accidental concomitants of putrescence, but now shown by Pasteur to be its essential cause, resolving the complex organic compounds into substances of simpler chemical constitution, just as the yeast-plant converts sugar into alcohol and carbonic acid.
His second paper on the antiseptic method appeared in both the British Medical Journal and the Lancet for 21 September 1867. In this article, entitled “On the Antiseptic Principle in the Practice of Surgery”, he discussed the rationale for and technical details of the method, and concluded with the following description of its “salubrious” effect on the hospital environment.
There is, however, one point more that I cannot but advert to, viz., the influence of this mode of treatment upon the general healthiness of an hospital. . . . (S)ince the antiseptic treatment has been brought into full operation, and wounds and abscesses no longer poison the atmosphere with putrid exhalations, my wards, though in other respects under precisely the same circumstances as before, have completely changed their character; so that during the last nine months not a single instance of pyemia, hospital gangrene or erysipelas has occurred in them.
As there appears to be no doubt regarding the cause of this change, the importance of the fact can hardly be exaggerated.
It was thus, with characteristic understatement, that Lister ushered in a new era in the prevention and control of surgical infection – and, by inference, indicted microorganisms as agents of other types of infection.
Lister’s first paper on the antiseptic method referred to above reported a series of 10 patients with compound fractures who fared much better under the antiseptic treatment than might have been expected under the usual care. However, more than such “anecdotal” information was needed to convince the sceptics among his surgical colleagues, of whom there were many. By 1870 Lister, who left Glasgow in 1869 to become Professor of Surgery at Edinburgh, had marshaled the evidence his thesis needed for its wider acceptance. In a paper in the Lancet “On the Effects of the Antiseptic System of Treatment upon the Salubrity of a Surgical Hospital”, he analyzed the outcome of amputations at Glasgow Infirmary before and after adoption of the antiseptic system. In 1864 and 1866, before adoption of the system, there were 35 amputations with 16 deaths for a mortality rate of 46%. in 1867, ’68 and ’69, after adoption of the system, there were 40 amputations with 6 deaths for a mortality rate of 15 %. This was a spectacular improvement in the mortality rate from amputation over that reported from leading British hospitals at the time.
For over a decade many leading British surgeons failed to recognize the merit of the antiseptic system, and much acrimonious criticism was directed at Lister and his method. When he visited the United States in 1876 to deliver an address at the International Medical Congress in Philadelphia, he was not received with any enthusiasm. The Americans were slow to accept Listerism, and as late as the meeting of the American Surgical Association in 1882, the Lancet reported that “Anti-Listerians were in the majority; . . . they relied for support upon the statements of others. . . . Surely it is too late in the day (for them) to contest the truth of the germ theory.” Levi Cooper Lane, who began his surgical career prior to Listerism, never fully accommodated to the restrictions imposed by the antiseptic and aseptic methods and gave as the reason: “You can’t teach an old dog new tricks.”
However, in Britain and on the continent, the antiseptic method had by 1879 been widely applied, and Lister’s findings amply confirmed. In that year Lister attended the International Congress of Medical Science at Amsterdam where his reception was far different from that he received from the Americans. When he rose to deliver his address, he was greeted by an overwhelming ovation that only abated when the President of the Congress came forward to take his hand and say:
Professor Lister, it is not only our admiration which we offer to you; it is our gratitude, and that of the nations to which we belong.
Lister’s work was the first convincing application of the germ theory to the control of human disease, and as such it spurred great progress in surgery and other fields. “There is no instance in the history of surgery, and indeed few in the history of science, in which a deduction has been so completely verified when put to the test.”
It soon became apparent that it would be more efficient to prevent wound contamination by sterilizing in advance all the drapes, dressings, gowns and instruments coming into contact with the operative field – thus creating an “aseptic” environment for the wound. This became feasible when Ernst von Bergmann (1836-1907), Professor of Surgery at Berlin, introduced steam sterilization in 1886 and inaugurated the present “aseptic” method in 1891. The procedures of aseptic surgery have now evolved over the past century to an elaborate standardized routine, including face masks, rubber gloves and laminar air flow; and, instead of carbolic acid, employing a broad spectrum of less noxious bactericidal antiseptics. The current regime, a combination of aseptic and antiseptic technology, is highly effective in barring live microorganisms from the wound – which is, in essence, the goal defined originally by Lister in 1867.
With the contributions of Lister, three essential pillars of modern surgery – anatomy, anesthesia and antisepsis/asepsis – were now in place. When the risk of surgical infection was reduced to a minimum by application of the Listerian principle, the domain of surgery expanded immediately to include bones and joints, body cavities, and vascular and other systems, a progression that continues to this day.
Robert Koch (1843-1910)
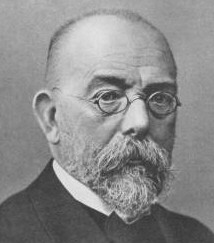
Robert Koch, native of Hannover, Germany, was the co-founder with Pasteur of the new field of bacteriology. Whereas Pasteur was a chemist who became a microbiologist and immunologist, Koch was a practicing physician who became the world’s preeminent bacteriologist and investigator of infectious diseases. Following a medical degree in Göttingen in 1866 and service in the Franco-Prussian War, Koch was appointed district physician at Woolskin where he combined his country practice with microscopic studies.
He began by working out the complete life-history and sporulation of the anthrax bacillus, and proving it to be the cause of the disease. When he demonstrated his culture methods and results to a group of well-known scientists at the Breslau Botanical Institute in 1876, they declared his discovery to be the greatest yet made in bacteriology.
Koch’s many other remarkable contributions to the creation of a new science included identification of the specific microbial agents responsible for two of humanity’s greatest plagues: the tubercle bacillus in 1882 and the cholera vibrio in 1883. His paper on the tubercle bacillus contains the first statement of the steps necessary to establish the pathogenic nature of a given microorganism, steps now known as “Koch’s postulates.” His elegant techniques of staining and culturing, and his historic discovery of two of the world’s most dangerous pathogens, coupled with his other wide-ranging scientific efforts, settled with finality the question of the microbiologic origin of infectious disease and earned for him the Nobel Prize in 1905.
By verifying the germ theory , the work of Pasteur, Lister and Koch ushered in the Golden Era of Microbiology which began with a phenomenal surge in research activity that shows no sign of abating to the present day. The search for causative organisms of specific diseases dominated the three decades from 1870 to 1900 and was highly successful. More than 20 pathogenic bacteria causing specific human diseases were identified, including:
| Date | Disease | Organism | Discoverer |
|---|---|---|---|
| 1868 | Leprosy | Mycobacterium leprae | Hansen |
| 1878 | Furuncule (Boil) | Staphylococcus | Pasteur |
| 1879 | Puerperal Fever | Streptococcus | Pasteur |
| 1879 | Gonorrhea | Gonococcus | Neisser |
| 1880 | Typhoid Fever | Salmonella typhi | Eberth |
| 1882 | Tuberculosis | Mycobacterium tuberculosis | Koch |
| 1883 | Cholera | Vibrio cholera | Koch |
| 1883 | Diphtheria | Corynebacterium diphtheriae | Klebs |
| 1884 | Tetanus | Clostridium tetani | Nicolaier |
| 1886 | Pneumonia | Pneumococcus | Fraenkel |
| 1887 | Meningitis | Meningococcus | Weichselbaum |
| 1892 | Gas Gangrene | Clostridium welchii | Welch |
| 1894 | Bubonic Plague | Pasturella pestis | Kitasato |
| 1898 | Dysentery | Shigella shigae | Shiga |
The predecessors to Stanford Medical School – Medical Department of the University of the Pacific, Medical College of the Pacific and Cooper Medical College – all evolved between 1850 and 1900. Medicine made more progress during this period than during any previous half century in the history of the world. In later chapters we shall see how these predecessor schools responded to the remarkable changes in medicine and medical education then in progress, and how they acquired the resources and programs that assured a smooth transition to Stanford auspices in 1908.
 Pasteur Brewing Louis Pasteur – Science, Health, and Brewing
Pasteur Brewing Louis Pasteur – Science, Health, and Brewing